About 20% of the European population will tell you they do experience chronic pain every day (Breivik et al., 2006). Despite the high level of knowledge on pain treatments, treatment strategies and pharmacology, more and more ‘alternative treatment options’ are popping up, such as acupuncture, hypnosis, biofeedback etc. Some authors refer to these treatment options as complementary medicine, which means that those treatment options are not considered to be part of conventional medicine (Deng & Cassileth, 2013). These treatments aim to focus on decreasing pain intensity, as well as emotional suffering, beliefs about pain and the behavioural component of pain, which all contribute to the patient’s pain experience (Jensen et al., 1991).
In this blogpost, we will focus on hypnosis and its application in the treatment of chronic pain. Hypnosis can be defined as a social interaction in which one person (the individual) responds to suggestions offered by another person (the hypnotist) for experiences involving alterations in perception, memory and voluntary action (Kihlstrom, 1985). It is sometimes considered as sleeping, but there are differences in brain activity patterns when sleeping or when being under hypnosis. The feeling of hypnosis can be approximated by driving in your car, and afterwards you do not remember certain parts of your scheduled route (cfr. driving on automatic pilot).
Dillworth et al. (2012) reviewed the application of hypnosis for chronic pain. During a session of hypnosis, about 70% of the individuals with chronic pain are able to experience a short-term reduction in chronic pain. In about 20-30% of the individuals, more permanent pain reductions in daily living were obtained. It is suggested, however, that the efficiency depends on the type of pain. Neuropathic and vascular pain would be more appropriate than for example low back pain.
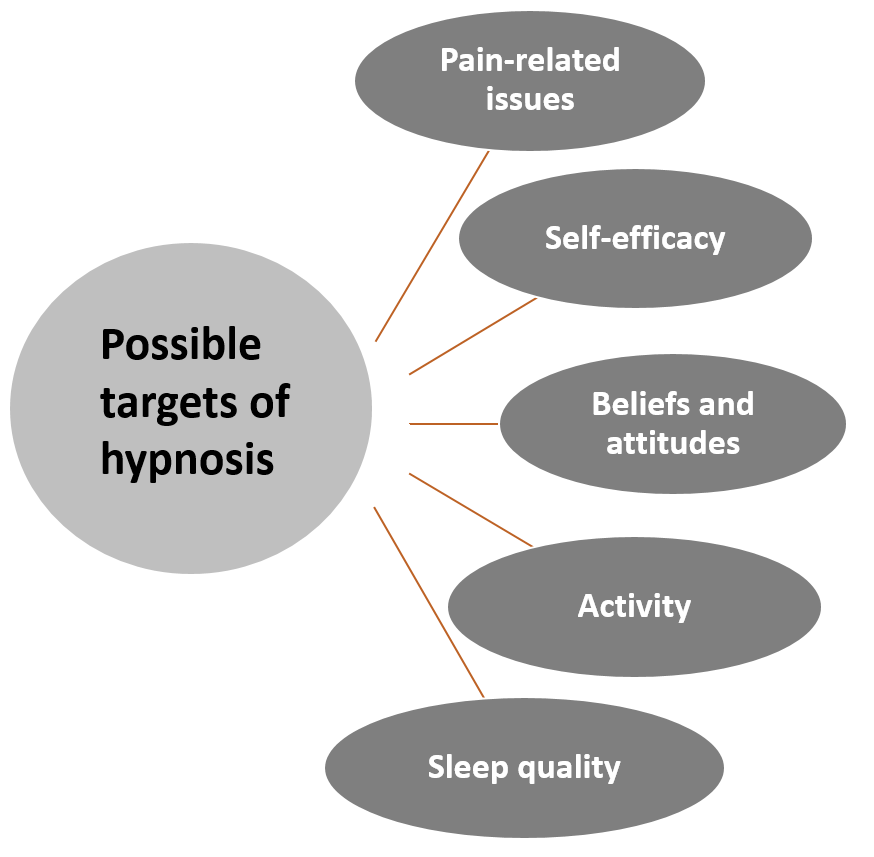
Hypnosis can be used as stand-alone treatment or in combination with for example cognitive behavioural therapy (CBT). In the latter, hypnosis has shown to enhance the efficacy of CBT. Several suggestions can be provided under hypnosis, whereby the focus is highly individual. Suggestions can target a range of pain-related outcomes among which pain reduction, attention shifts, changing pain sensations, increased comfort etc. It is advised to use a variety of suggestions, based on sensory, affective, cognitive and motivational components. Furthermore, it is also possible to use self-hypnosis, enhancing the cost-effectiveness of hypnosis (Dillworth et al. 2012).
Aveni et al. (2016) evaluated the attitudes of 1247 healthcare professionals regarding complementary medicine (CM) at a university hospital in Switzerland. Overall, 96.1% agreed that CM could be useful for the treatment of chronic pain. Hypnosis, osteopathy and acupuncture were the three therapy options that were the most favoured by the medical staff. Although the positive attitudes of the healthcare professionals, they do not recommend it spontaneously to patients. In total 84.3% felt lack of knowledge to inform their patients about CM. As a conclusion, it can be stated that professionals are not opposed to using non-conventional therapies. There is only a lack of expert knowledge about those treatment options that prevents them from proposing it to patients. [IB1]
These articles highlight the importance of complementary medicine in treating chronic pain patients. Although healthcare providers will not always mention other treatment options, it does not mean they have opposite ideas about it. Hypnosis is one of those options with minimal side effects which can be explored when conventional treatments are not sufficient enough to reduce either the pain intensity or either the complete pain experience including the affective, cognitive and behavioural component.
Lisa Goudman
Lisa Goudman is a PhD researcher at the University of Brussels and is a member of the Pain in Motion research group.
2018 Pain in Motion
Poll
What is your opinion regarding complementary and alternative medicine in healthcare?
Give your opinion on https://goo.gl/kXvCFY
Follow the results on https://goo.gl/4PNvGa
References and further reading:
Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287-333.
https://www.ncbi.nlm.nih.gov/pubmed/16095934
Deng G & Cassileth B. Complementary or alternative medicine in cancer care—myths and realities. Nature Reviews Clinical Oncology. 2013;10:656–664. https://www.nature.com/articles/nrclinonc.2013.125
Jensen MP, Turner JA, Romano JM, Karoly P. Coping with chronic pain: a critical review of the literature. Pain. 1991;47(3):249-83.
https://www.ncbi.nlm.nih.gov/pubmed/1784498
Kihlstrom JF. Hypnosis. Annu Rev Psychol. 1985;36:385-418. https://www.ncbi.nlm.nih.gov/pubmed/3883892
Dillworth T, Mendoza ME, Jensen MP. Neurophysiology of pain and hypnosis for chronic pain. Transl Behav Med. 2012;2(1):65-72. https://www.ncbi.nlm.nih.gov/pubmed/24073099
Aveni E, Bauer B, Ramelet AS, Kottelat Y, Decosterd I, Finti G, Ballabeni P, Bonvin E, Rodondi PY. The Attitudes of Physicians, Nurses, Physical Therapists, and Midwives Toward Complementary Medicine for Chronic Pain: A Survey at an Academic Hospital. Explore (NY). 2016;12(5):341-6.
https://www.ncbi.nlm.nih.gov/pubmed/27450407
[IB1]Deze alinea gaat dan wel weer over CM in het algemeen…