The biomedical model falls short in explaining chronic pain. Although many clinicians have moved on in their thinking and apply a broad biopsychosocial view with regard to chronic pain (patients), the majority of clinicians (including myself) have received a biomedical-focused (undergraduate) training/education. We know from a series of studies that such a biomedical training is likely to influence the therapists’ attitudes and core beliefs towards chronic pain. Yet few therapists are aware of the impact their own attitudes and beliefs have on the patient, and probably those who are aware of this, adopt a broader biopsychosocial view. Those unaware are probably bored with this biopsychosocial model – they probably never achieved of thorough understanding of the model or use excuses (e.g., I use the ICF as a framework for my assessments) to cover-up their pure biomedical (treatment) focus.
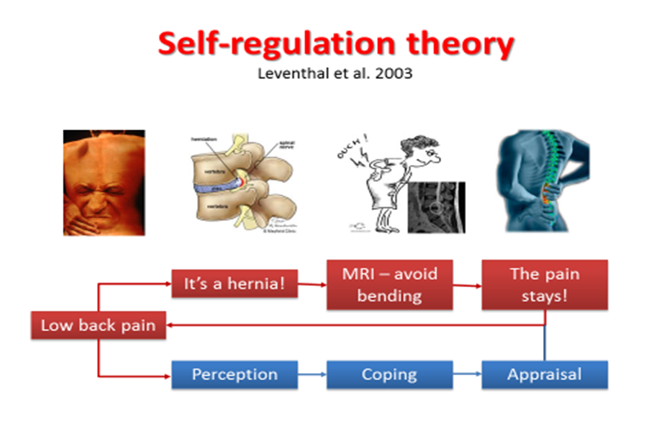
More specifically, the therapist’s attitudes and beliefs influence the patient’s attitudes and beliefs. In case the therapist holds strong biomedical beliefs regarding chronic pain, the patient will adopt these beliefs accordingly. Typical examples of such biomedical beliefs include: pain is related to tissue damage; chronic low back pain is due to spinal instability or an injured intervertebral disc; lifting of heavy objects with poor posture is dangerous for the lumbar spine; patients with whiplash associated disorders suffer big time – there must be something wrong with them and it must be located in the cervical spine or the head. The self-regulation theory by Leventhal et al. (2003) provides an excellent conceptual framework for explaining how patients’ (and therapists’) beliefs influence their behavior (the figure below illustrates this).
As patient’s attitudes and beliefs influence treatment adherence, therapists should be aware that focusing on the biomedical model for chronic musculoskeletal pain is likely to result in poor compliance with evidence based treatment guidelines, less treatment adherence and a poorer treatment outcome. The starting point for preventing such a poor outcome entails self-reflection. For instance, evidence from published randomized controlled trials addressing rehabilitation of chronic musculoskeletal pain has revealed that self-efficacy, depression, pain catastrophizing and physical activity should be the primary treatment targets for patients with chronic musculoskeletal pain. Are those the 4 main treatment targets in our treatments for patients with chronic pain? Therapists learning about more up-to-date understanding and treatments for patients with chronic pain often say (or think) that it is very difficult to change the patients’ behavior. In our experience this can be the case in selected cases, but the majority of patients are ‘manageable’. The therapists however, especially those having many years of clinical experience, are often more difficult to ‘teach’.
Once the therapist holds evidence-based attitudes and beliefs regarding chronic pain, assessing patients’ attitudes and beliefs will likely become the natural next step in their changing behavior as therapists (if this ever occurs of course). If they do, they can easily integrate the information regarding the patients’ attitudes and beliefs (including illness perceptions) in the clinical reasoning process, which in turn results in individually-tailored treatment programs that specifically address the patients’ attitudes and beliefs in order to improve treatment adherence and outcome. This is a lot of fun and prevents boring ‘standard’ treatment programs (boring for the therapist especially!). It’s a lot of fun because challenging the patients’ maladaptive attitudes & beliefs is typically an unpredictable therapeutic challenge, but one that is very rewording in the end and also very inspiring. It’s a unique avenue, every single time! Enjoy it!
Jo Nijs
2016 Pain in Motion
References and further reading:
Nijs J, Roussel N, Paul van Wilgen C, Köke A, Smeets R. Thinking beyond muscles and joints: therapists' and patients' attitudes and beliefs regarding chronic musculoskeletal pain are key to applying effective treatment. Man Ther. 2013 Apr;18(2):96-102.
https://www.ncbi.nlm.nih.gov/pubmed/23273516
Domenech J, Sánchez-Zuriaga D, Segura-Ortí E, Espejo-Tort B, Lisón JF. Impact of biomedical and biopsychosocial training sessions on the attitudes, beliefs, and recommendations of health care providers about low back pain: a randomized clinical trial. Pain. 2011 Nov;152(11):2557-63.
https://www.ncbi.nlm.nih.gov/pubmed/21917377
Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain. 2012 Jan;16(1):3-17.
https://www.ncbi.nlm.nih.gov/pubmed/21719329
van Wilgen P, Beetsma A, Neels H, Roussel N, Nijs J. Physical therapists should integrate illness perceptions in their assessment in patients with chronic musculoskeletal pain; a qualitative analysis. Man Ther. 2014 Jun;19(3):229-34.