Pain has always been a matter of interest to those involved in rehabilitation and medicine. Decades of research has led to the understanding that pain is an extensive and complex mechanism, influenced by thoughts, emotions, context, previous experiences, perceptions, etc. Therefore, pain logically goes beyond the presence of tissue damage and can even occur without it.
Many chronic pain patients show signs of generalised hypersensitivity, often called central sensitization. This is characterized by increased neuronal responsiveness, increased nociceptive processing, malfunctioning of endogenous descending nociceptive modulation and abnormalities in brain structure, function and chemistry. These characteristics are believed to be reversible when using efficient therapy modalities, but to date the clinical relevance of these advances in modern pain neurosciences seems limited to the general adult musculoskeletal pain population. However, evidence arises that also post-cancer, pediatric and sport-related pain patients might benefit from a treatment approach based on modern pain neurosciences, as evidence for the presence of central sensitization in (at least a part of) these patients is increasing.
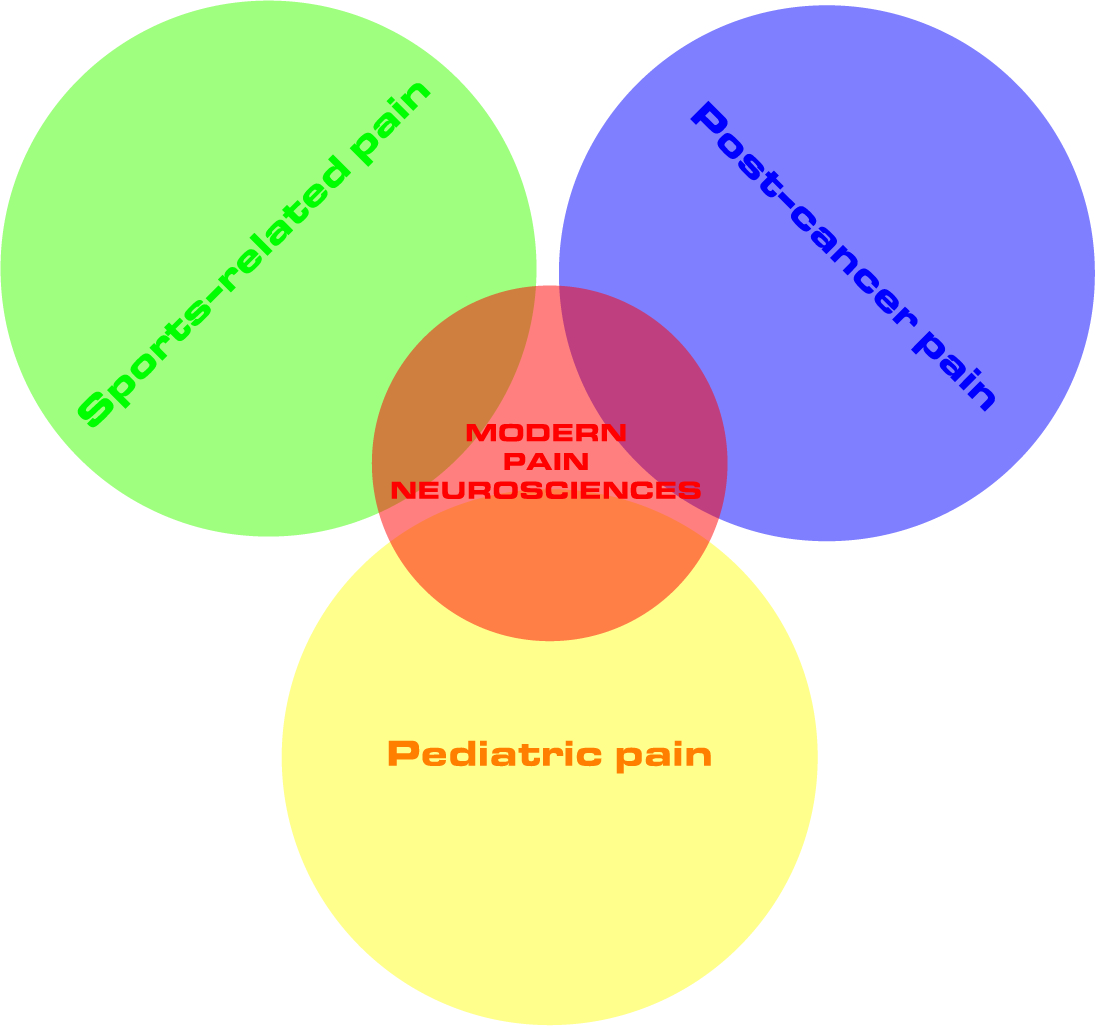
The use of a classification system based on the dominant pain type might therefore not only apply to the adult musculoskeletal pain population, but can also be useful in patients with post-cancer, pediatric and sport-related pain. The differentiation between predominant central sensitization pain, neuropathic or nociceptive pain is relevant for clinical practice since neuropathic and mixed pain types are thought to be more difficult to treat than nociceptive pain. This pain mechanism-based approach could lead to more patient-centred care, by recognizing the unique personal experience of pain. Together with the classification of the predominant pain type, modern pain neurosciences offer a broad perspective of treatment modalities within the field of physiotherapy, including education, stress management, sleep management, exercise interventions, etc.
Regarding the populations discussed here, stress might be a relevant point of action. Whereas pediatric pain patients might suffer from stress due to (repetitive) medical interventions, athletes might endure a lot of stress or pressure to perform. Post-cancer pain patients on the other hand typically suffer from prolonged emotional and physical stress due to the diagnosis of cancer and its related treatment. While stress is able to relieve pain in healthy persons, chronic pain patients often suffer from an inadequate stress response, which increases the usefulness of implementing stress management and relaxation techniques in the treatment program, given the lack of medical treatment for this problem.
Additionally, the use of physical activity and exercise programs in the management of patients with pediatric, post-cancer or sport-related pain problems should be emphasized. Exercise programs should however be adapted to modern pain neuroscience knowledge and aim at changing coping strategies, pain perceptions and beliefs, fears and other counterproductive psychosocial factors. Given the importance of physical activity and exercises in the general population and the chronic pain population in particular, it should be the responsibility of the physical therapist to provide ideal conditions for its implementation in these patients (e.g. preparing the patient for physical activity and exercises by delivering pain neuroscience education in order to tackle possible disadvantageous factors).
Anneleen Malfliet
Member of the international Pain in Motion research group.
PhD researcher at Vrije Universiteit Brussel, Brussels, Belgium.
Funded by the Research Foundation Flanders (FWO), Belgium.
2017 Pain in Motion
References and further reading:
Malfliet A, et al. Modern pain neuroscience in clinical practice: Applied to post-cancer, pediatric and sports-related pain. BJPT; 2017: paper accepted for publication.
Fernandez-Lao C, et al. Widespread mechanical pain hypersensitivity as a sign of central sensitization after breast cancer surgery: comparison between mastectomy and lumpectomy. Pain Med; 2011;12(1):72–8.
https://www.ncbi.nlm.nih.gov/pubmed/21143767
Duarte MA, et al. Pressure pain threshold in children with recurrent abdominal pain. J Pediatr Gastroenterol Nutr.; 2000;31(3):280–5.
https://www.ncbi.nlm.nih.gov/pubmed/10997373
Cornelissen L, et al. Pain hypersensitivity in juvenile idiopathic arthritis: a quantitative sensory testing study. Pediatr Rheumatol Online J.; 2014;12:39.
https://www.ncbi.nlm.nih.gov/pubmed/25249820
Plinsinga ML, et al. Evidence of Nervous System Sensitization in Commonly Presenting and Persistent Painful Tendinopathies: A Systematic Review. J Orthop Sports Phys Ther.; 2015;45(11):864–75.
https://www.ncbi.nlm.nih.gov/pubmed/26390275
Martenson ME, et al. A possible neural basis for stress-induced hyperalgesia. Pain.; 2009;142(3):236–44.
https://www.ncbi.nlm.nih.gov/pubmed/19232470
Pedersen BK & Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scand J Med Sci Sports.; 2006;16 Suppl 1:3–63.