In this blogpost, the most important elements of this systematic review and meta-analysis are highlighted:
“Ancient pain theory in the age of Aristotele suggested that pain is perceived by the soul that is located in the heart. Linton noted that in those days, “the brain was not believed to have any direct influence” and that “for years the heart was considered to be the center for pain sensation.” While nowadays the fact that nociceptive information is processed in the brain, and the sensation of pain is related to brain function is indisputable, some of the ancient ideas still hold truth.
An important structure linking cardiovascular and pain regulatory systems is the pneumogastric nerve – the vagus.
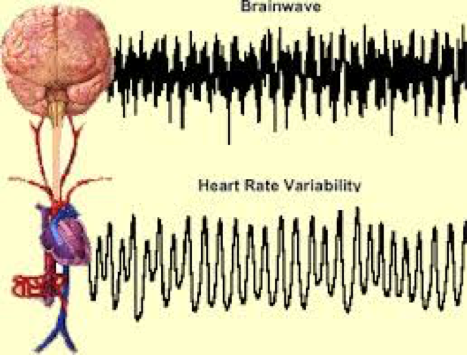
The influence of the vagus nerve on these (acute) nociceptive processes can be described at different levels of the nociceptive pathway. At the level of spinal nociceptive transmission, early experimental work in rats established that the experimental activation of vagal afferent fibers by electrical stimulation could facilitate or inhibit responses of dorsal horn neurons to noxious heating of the skin . The authors concluded, that “the role of vagal afferents in nociception may be interpreted in two ways: facilitation of the perception of relevant stimuli, which is beneficial to the organism, and inhibition of nociceptive transmission via linkage with known endogenous pain control systems” . We will return to this idea later; however, it is important to note that this network is bi-directional and also links to descending inhibitory pathways from cerebral structures to the dorsal horn. These descending pathways are capable of suppressing or potentiating the processing of nociceptive information in addition to the ascending pathways (vagal afferents) involved in transducing noxious stimuli to the central branches (presynaptic terminals in the spinal cord). This descending inhibition is relayed via the nucleus tractus solitarius (NTS) that receives major input from the vagus nerve and thus represents the initial relay for descending vagally mediated nociceptive effects. As a consequence of impaired vagal control , the descending control within the spinal cord dorsal horn may be disrupted and contribute to the central sensitization increasing the excitability of neurons in the central nervous system (CNS) in chronic pain . Decreased vagal activity may therefore result in greater somatic and visceral input via the spinothalamic tract, which in turn provides a mechanism for decreased pain threshold and increased pain sensitivity in those with chronic pain. On the other end of this chain and related to the autonomic outflow, sympathetic and parasympathetic preganglionic nuclei in the spinal cord receive input from descending inhibitory pathways . These preganglionic nuclei influence pain thresholds and modify autonomic outflow by baroceptor-mediated changes in arterial pressure leading to well described phenomena characterized by alterations in the nociception of acute painful stimuli (i.e., hypertension-related hypoalgesia) . Blood pressure and heart rate (HR) – both products of the ANS – have been widely studied in investigations of the relationship between acute pain stimuli and autonomic reactions.
Within the present meta-analysis we aimed to investigate differences in vmHRV between CPPs and HCs. After an extensive search of the literature, we identified 55 studies that were eligible for inclusion based on predefined inclusion criteria. Included studies yielded a total of 86 comparisons of time- and frequency-domain measures of vmHRV. Within the following paragraphs, we will summarize our results and discuss the implications as well as potential underlying mechanisms of the present findings.
Chronic pain patients have lower vagal activity indexed by measures of vmHRV compared to HCs. Exploring the potential mechanism underlying these findings and discussing the implications of our results, we provided evidence for (i) a role of the vagus nerve in spontaneous pain processing at the level of nociceptive transmission to the brain, (ii) highlighted shared neural networks underlying this association, referred to (iii) a model of neurovisceral integration in pain processing that links physiology to psychological concepts of interest in the study of chronic pain (i.e., comorbidities), and reviewed (iv) alterations in brain morphology in CPPs related to brain regions that are commonly associated with HRV, providing a rational why vagal activity, indexed by HRV, is altered in CPPs. We briefly discussed the vagus nerve as a target and outcome of manifold therapeutic interventions in chronic pain patients and provided suggestions for future research. It is hoped that this review will stimulate further research in this important area of CP research.”
Yannick Tobbackx
2016 Pain in Motion
References and further reading:
Koenig J, Falvay D, Clamor A, Wagner J, Jarczok MN, Ellis RJ, Weber C, Thayer JF. Pneumogastric (Vagus) Nerve Activity Indexed by Heart Rate Variability in Chronic Pain Patients Compared to Healthy Controls: A Systematic Review and Meta-Analysis. Pain Physician. 2016 Jan;19(1):E55-78. Review.
http://www.ncbi.nlm.nih.gov/pubmed/26752494
Free PDF available from: