Within the biomedical model, pain is considered a consequence of tissue damage. However, we all know now that a precise biomedical diagnosis cannot be given in the majority of the low back pain (LBP) patients. Enter: the biopsychosocial perspective.
Various factors, often referred as yellow flags, enhance the complaints and contribute to the development of chronic LBP (CLBP). Inappropriate illness perceptions have been associated with the development of exaggerated pain and higher levels of disability. A patient’s behaviour is influenced to a considerable degree by these cognitions and emotions. The illness perceptions of patients with CLBP will determine their prognosis: patients who attribute more symptoms to their disease, who expect their problem to last a long time or who believe they have little control over their complaints, show a poorer outcome in 6 months. Furthermore, illness perceptions in CLBP do not only help to determine the clinical effect of treatment, but also the adherence to the interventions. Because if I believe that only rest will cure my pain, why would I ‘work my butt of’ with home exercises??
So what you see, is what you get … or maybe you remember something about self-fulfilling prophecies in a long lost past…
But hey, don’t blame it all on the patient! The therapist is to blame too, you know. Because his/her perceptions (we call it ‘attitudes and beliefs’) are equally determining their behaviour. Studies on attitudes and beliefs of health care practitioners (HCPs) confirm that the prescription behaviour is determined by the beliefs about the complaint. There appears to be a difference in prescription behaviour between HCPs with a biomedical or a biopsychosocial background. Most HCPs with a biomedical background have a prescription behaviour that is not in line with the evidence based guidelines of CLBP. This has been investigated to a limited extend in physicians, physiotherapists and students (UK, Brasilia and Australia), but not in our region.
Aha, that’s where we enter!
Since perceptions are socially-culturally determined and education of HCPs differs enormously between countries, we thought it would be relevant to examine these attitudes and beliefs in Belgium and the Netherlands and to link them with the adherence to clinical guidelines. As a sneak preview I will give you the results of 1624 physiotherapy students (as they are the future!).
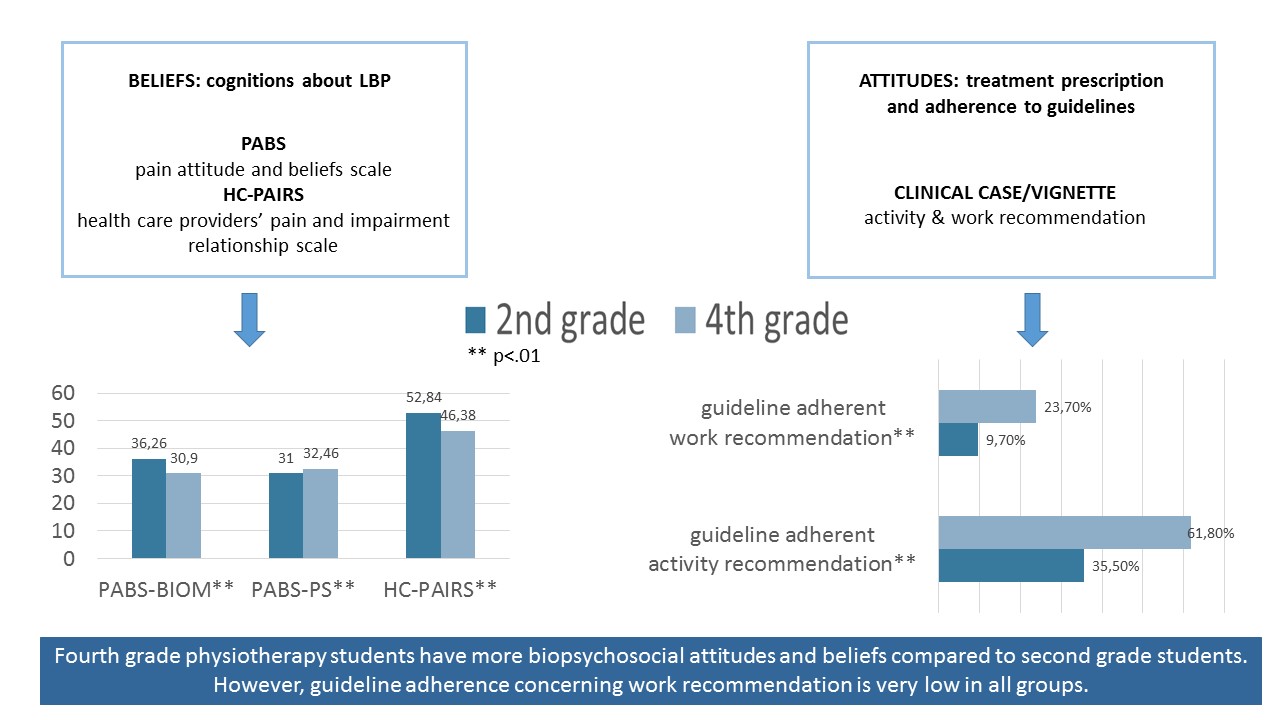
We saw that 4th grade students have a more biopsychosocial belief and attitude towards CLBP compared to 2nd grade students (hooray!). However, guideline adherence concerning activity and work recommendations remains low in all students. Really, brace yourselves: only 47% (activity recommendations) and 16% (work recommendations) of the students answered according to the current evidence based clinical guidelines. Isn’t that sad? Isn’t that alarming? Where does this come from? Where are we going wrong? No way the patient is (the only one) to blame!
There you have it… you ain’t seen nothing yet.
So can I ask you a question now? Why do you personally think there is a lack of guideline adherence in students?
Give your opinion: https://goo.gl/rcLYWg
Follow the results: https://goo.gl/VV9GL0
Marijke Leysen
Marijke Leysen is working on a joint PhD (UAntwerpen and VUB) about the attitudes and beliefs concerning low back pain.
2017 Pain in Motion
References and further reading:
Bishop A, Foster NE, Thomas E, Hay EM: How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health care practitioners? A survey of UK general practitioners and physiotherapists. Pain 2008, 135(1-2):187-195.
https://www.ncbi.nlm.nih.gov/pubmed/18206309
Domenech J, Sanchez-Zuriaga D, Segura-Orti E, Espejo-Tort B, Lison JF: Impact of biomedical and biopsychosocial training sessions on the attitudes, beliefs, and recommendations of health care providers about low back pain: a randomised clinical trial. Pain 2011, 152(11):2557-2563.
https://www.ncbi.nlm.nih.gov/pubmed/21917377
Foster NE, Bishop A, Thomas E, Main C, Horne R, Weinman J, Hay E: Illness perceptions of low back pain patients in primary care: what are they, do they change and are they associated with outcome? Pain 2008, 136(1-2):177-187.
https://www.ncbi.nlm.nih.gov/pubmed/18313853
Houben RM, Ostelo RW, Vlaeyen JW, Wolters PM, Peters M, Stomp-van den Berg SG: Health care providers' orientations towards common low back pain predict perceived harmfulness of physical activities and recommendations regarding return to normal activity. European journal of pain (London, England) 2005, 9(2):173-183.
https://www.ncbi.nlm.nih.gov/pubmed/15737810
Leysen M, Nijs J, Meeus M, Van Wilgen P, Struyf F, Vermandel A, Kuppens K, Roussel N. Clinimetric properties of IPQ-R and Brief IPQ in patients with musculoskeletal disorders: A systematic review. Manual Therapy 2015 Feb;20(1):10-7.