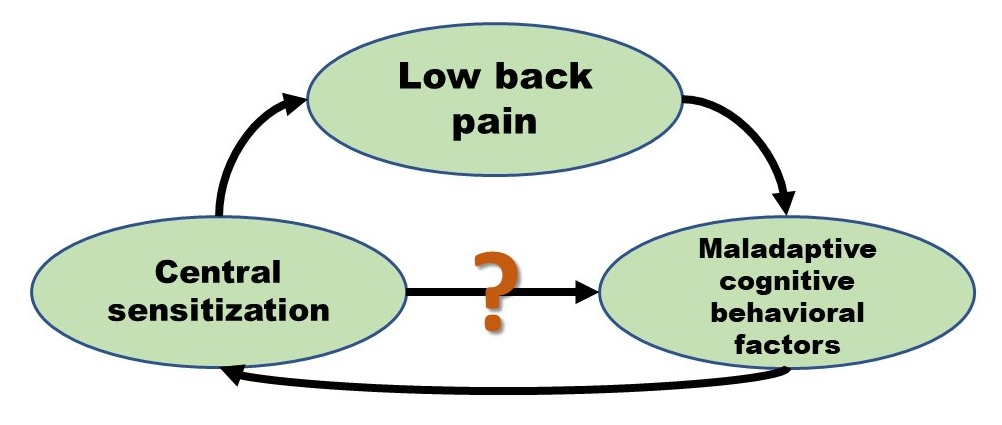
Chronic low back pain (CLBP) is a major problem in today’s society, and often no specific medical cause can be found for the patient’s complaints. Modern pain neurosciences confirmed that the involvement of central sensitization (CS) might explain the patient’s pain and symptoms (Nijs et al. 2015, Nijs et al. 2014). However, it remains unclear why only subgroups of patients show CS. It has been suggested that psychosocial and cognitive behavioral factors such as depressive feelings, pain catastrophizing and fear avoidance behavior might play a role in the development and maintenance of CLBP (Roussel et al. 2013). Therefore a recent study by our research group aimed at investigating the relationship between CS and cognitive behavioral factors (n=38)(Huysmans et al. 2018).
It was found that scores on the Central Sensitization Inventory (Neblett et al. 2013), measuring the presence of symptoms of CS, correlated significantly with pain behavior, pain intensity, illness perceptions, kinesiophobia and pain catastrophizing. Furthermore, patients showing a clinically relevant degree of symptoms of CS, had significantly worse scores on outcomes measuring pain catastrophizing, pain intensity, kinesiophobia, pain behavior and illness perceptions, compared to those having less symptoms of CS (n=26). These relationships have been studied and confirmed in other populations. In patients with knee osteoarthritis, for example, it was found that higher levels of CS were associated with increased pain catastrophizing, low sleep efficiency and high levels of pain experience (Campbell et al. 2015). CS also led to more anxiety, depressive feelings, pain, fear avoidance behavior and poorer sleep quality in patients with chronic trapezius myalgia.
Furthermore, our study affirmed the already known phenomenon that in contrast to other populations, such as fibromyalgia and chronic fatigue syndrome, in which CS is dominantly present, CS only occurs in subgroups of patients with CLBP (Nijs et al. 2010, Smart et al. 2012). A possible explanation might be the popular ‘fear-avoidance-model’, which is a model that explains the role of psychosocial factors in the development of chronic pain (Vlaeyen et al. 2000, Leeuw et al. 2007). The model theorizes that during a pain episode, some patients develop pain catastrophizing, which leads to fear avoidance behavior, resulting in more disability and eventually chronic pain.
Our and previous findings regarding this matter underscore the fact that psychosocial and cognitive behavioral factors could contribute to and sustain the mechanism of CS, and these relations may be bidirectional. One could therefore assume that CS affects and is affected by pain cognitions and perceptions, resulting in a vicious circle leading to chronic pain and disability. This assumption may add a more biopsychological level to the onset and maintenance of CS dominated chronic low back pain.
Eva Huysmans
2018 Pain in Motion
References and further reading:
Nijs J, Apeldoorn A, Hallegraeff H, et al. Low back pain: guidelines for the clinical classification of predominant neuropathic, nociceptive, or central sensitization pain. Pain Physician 2015; 18(3): E333-46.
https://www.ncbi.nlm.nih.gov/pubmed/26000680
Nijs J, Torres-Cueco R, van Wilgen CP, et al. Applying modern pain neuroscience in clinical practice: criteria for the classification of central sensitization pain. Pain Physician 2014; 17(5): 447-57.
https://www.ncbi.nlm.nih.gov/pubmed/25247901
Roussel NA, Nijs J, Meeus M, Mylius V, Fayt C, Oostendorp R. Central sensitization and altered central pain processing in chronic low back pain: fact or myth? Clin J Pain 2013; 29(7): 625-38.
https://www.ncbi.nlm.nih.gov/pubmed/23739534
Huysmans E, Ickmans K, Van Dyck D, et al. Association Between Symptoms of Central Sensitization and Cognitive Behavioral Factors in People With Chronic Nonspecific Low Back Pain: A Cross-sectional Study. Journal of manipulative and physiological therapeutics 2018.
https://www.ncbi.nlm.nih.gov/pubmed/29329739
Neblett R, Cohen H, Choi Y, et al. The Central Sensitization Inventory (CSI): establishing clinically significant values for identifying central sensitivity syndromes in an outpatient chronic pain sample. J Pain 2013; 14(5): 438-45.
https://www.ncbi.nlm.nih.gov/pubmed/23490634
Campbell CM, Buenaver LF, Finan P, et al. Sleep, Pain Catastrophizing, and Central Sensitization in Knee Osteoarthritis Patients With and Without Insomnia. Arthritis Care Res (Hoboken) 2015; 67(10): 1387-96.
https://www.ncbi.nlm.nih.gov/pubmed/26041510
Nijs J, Van Houdenhove B, Oostendorp RA. Recognition of central sensitization in patients with musculoskeletal pain: Application of pain neurophysiology in manual therapy practice. Man Ther 2010; 15(2): 135-41.
https://www.ncbi.nlm.nih.gov/pubmed/20036180
Smart KM, Blake C, Staines A, Doody C. Self-reported pain severity, quality of life, disability, anxiety and depression in patients classified with 'nociceptive', 'peripheral neuropathic' and 'central sensitisation' pain. The discriminant validity of mechanisms-based classifications of low back (±leg) pain. Man Ther 2012; 17(2): 119-25.
https://www.ncbi.nlm.nih.gov/pubmed/22074733
Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 2000; 85(3): 317-32.
https://www.ncbi.nlm.nih.gov/pubmed/10781906
Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 2007; 30(1): 77-94.